Medication expiry dates: What are the risks?
MITIGATING AGAINST THE RISKS OF EXPIRED MEDICATION AND FAULTY EQUIPMENT
For superyachts, medication and equipment has to work when needed, especially during a voyage or at sea.
In this blog we look at some of the risks around expired medication or faulty devices and how to mitigate against these.
The two biggest preventable influences on ‘drug and device’ longevity are temperature of storage, and frequency/way of handling.
TEMPERATURE
Every drug in a long-term kit is temperature stable (within reasonable temperature limits).
Drugs which are not temperature stable, can lose their efficacy when out of temperature range and so have to be stored in a refrigerator. Storing drugs like this without a 24/7 monitoring and alarm system to warn you about any temperature changes, can however give a false sense of security, as, they may be rendered ineffective without you knowing.
Example: Insulin - it’s not the changing of the chemical composition that makes people sick but the fact people expect it to still work and it doesn’t.
HANDLING OF MEDICATION AND DEVICES
The reasons for devices and medication to become dysfunctional when poorly handled range from:
- Less obvious situations: A sealed injection syringe inside its wrapper, being (mis)handled so many times that it is no longer sterile. This may also apply to sealed sterile dressings.
- Obvious situations: An AED or piece of equipment being dropped from a significant height.
- Common situations like (mis)handling leading to a lack of usefulness in a medical device and its contents: Opening a sealed liquid container such as eye irrigation or other eyedrops, contaminating the tip, then putting the cap back on and leaving it for the next person to potentially receive a transmitted secondary infection.
WHAT ARE THE RISKS CONCERNING BATTERY LIFE?
The most common reason why battery-powered medical devices don't work in an emergency, is because they have been overcharged (not because they have been discharged and not charged up again).
If you leave any battery-powered medical device plugged in continuously for months at a time, you are likely to find that it will usually work when you need it but for a much shorter time than advertised, because the battery capacity has been overstressed to the point where it is dysfunctional.
This is of course a generalisation but it's a frequent problem when we get emergency calls and is most frequent with cardiac monitors, defibrillators, and airway suction pumps – which you really don't want to fail when you need them.
With devices like oxygen concentrators, remember that the manufacturers’ battery life is optimistic (the complete reverse of drug shelf-life) and while in laboratory conditions a particular battery may run an oxygen concentrator for, say, four hours, in real life that very quickly deteriorates to 2/2-3 hours after multiple recharging cycles and a tough life of being carried around and bounced off various surfaces. This is also not manufacturer-dependent; these caveats apply to all such devices.
SO, WHAT ABOUT EXPIRY DATES?
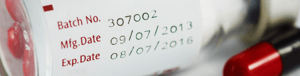
Since 1979, all drug manufacturers have been required to stamp an expiration date on their products. The date relates to when the manufacturer can still guarantee the full potency and safety of the drug.
Assuming recently stable pharmaceuticals are kept at a reasonably consistent temperature, stored out of direct sunlight, cool but not frozen, then they will almost certainly work well beyond the date put on the manufacturers package - clearly, a drug which expires October 2022 is not suddenly valueless and dangerous in the first week of November, but also the line has to be drawn sometime.
Some years ago, the Food and Drug Administration in the U.S. (not the manufacturers) conducted a study of drug shelf life at the request of the US military. The short summary is that of 100 drugs, both prescription and over-the-counter, 90% were perfectly good to use even 15 years after the expiration date, but 10% weren't.
It's true the effectiveness of a drug may decrease over time, but much of the original potency still remains even a decade after the expiration date. Excluding nitroglycerine, insulin, and liquid antibiotics, most medications are as long-lasting as the ones tested by the military and as mentioned, placing medication in a cool place (not just a temperate place), such as a refrigerator, prolongs drug longevity and will help a drug remain potent for many years.
Despite this, over time, medications break down into other chemicals which in very rare circumstances, could have an adverse effect on your body. Ultimately, once the package date is past - then for these reasons, as well as medicolegal reasons, we shouldn't use them unless in an emergency and only then after checking.
What's the take-home lesson?
The expiration dates are deliberately conservative to ensure you get the safety and the efficacy you expect and paid for.
Two key suggestions for yachts:
- Considering current supply chain difficulties (and as many of our yachting clients already do) make sure that you look to renew your drug stocks months in advance of their expiry dates.
- If you're a long way from resupply/port, don't throw out drugs coming up to the expiry date until you have them replaced because there may be a time where with appropriate medical advice, the patient may be better off to use a just-past-its-expiry-date drug, than have nothing at all.
Luckily MedAire clients have access to our Sea to Shore App, which makes managing your medical kit inventory and viewing any upcoming expiring medication an easy process.
FIND OUT MORE
For any product enquiries, reach out to your Account Manager or contact us here. If you have any medical questions, clients can contact MedLink.
